Image: created by Bahnijit Barman; altered by paramedmovement
Have you ever played Pokemon Go? Or maybe even seen the TV show? When I was young I would collect the cards, we would trade them and play the card game. We would buy new card packs hoping to find a high level pokemon! Rarely was that the case. Pokemon start out in their basic form and can evolve into a stronger version of themselves; this evolution usually can occur twice. With each evolution, the pokemon would gain more hit points or even a new ability.



Well, one day you'll grow out of that and focus on the more productive things in life........LIKE HOW TO EVOLVE YOUR STROKE EXAM! Our main goal when it comes to stroke care, in the prehospital environment, is two fold: identify the stroke and transport to the appropriate facility (primary VS thrombectomy capable VS comprehensive stroke center).
Basic Stroke Exam
Think way back to EMT school, what was the very first stroke exam you learned? For me it was the FAST and Cincinnati Prehospital Stroke Scale (CPSS). They were simple and easy to learn foundational exams. I went out into the field armed and ready to catch some strokes. My Paramedic partner would say "Hey Tyler go ahead and do a stroke exam." No problem, I would perform the exam and relay the findings to my partner. But every now and then my partner would do some additional exams. They would check grip strength, lower extremity weakness, and maybe even do a vision exam. I was intrigued and started asking questions. Come to find out there are as many stroke exams out there as pokemon: FAST, FAST-ED, MEND, BEFAST, CPSS, LAPSS, SLAMS, C-STAT. The list goes on. I am not going to debate which is best, that is not the focus of this blog. Pick one of these exams, this is the foundation that you will build on. So what is the next evolution?
Large Vessel Occlusion (LVO) Stroke Exam
As the name implies, we have several large vessels that supply the brain. When a patient experiences an occlusion of one of these vessels a significantly larger amount of brain tissue is at risk. Which vessels are we talking about here?
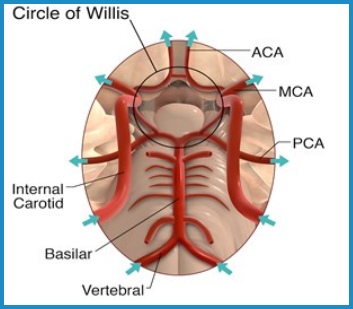

Images obtained from: University of North Carolina
Some of you may be lucky and have a hospital in your back yard that offers comprehensive stroke care. In this blog we will not cover all the different types of stroke care that hospitals provide (primary/comprehensive/thrombectomy capable). However, it is important to know that patients experiencing a LVO stroke have improved outcomes when they are transported to a comprehensive stroke center. These hospitals have the capability to perform mechanical thrombectomy (MT); a procedure that allows an interventional radiologist to physical retrieve the clot via specialized equipment.
How does MT compare to thrombolysis (tPA)? One study compared thrombectomy versus medically managed (tPA) LVO stroke patients and concluded, "Endovascular therapy was statistically associated with lower NIHSS at discharge (p=0.04), favorable NIHSS shift (p=0.03), and increased independence rates at discharge (p=0.03) and 3-6-month follow-up (p=0.04)" (Haussen et al., 2018). MT also has a longer treatment window and can be performed up to 24 hours from the onset of stroke. The DAWN trial, "is the first randomized investigation of endovascular intervention versus standard treatment for AIS due to anterior circulation LVO beyond 8 h of onset (Starke et al., 2018)." They found that, "Significant clinical benefit was seen in patients who received endovascular intervention compared with standard medical therapy (utility-weighted mRS 5.5 vs 3.4). Furthermore, 90-d functional independence was 49% in the thrombectomy group versus 13% in the control group (Starke et al., 2018)."
What if we had a stroke exam that could help us determine who is having a LVO stroke. We do! In fact there are several stroke scale/exams utilized for this. I am going to talk about one simple easy to use exam, the VAN!
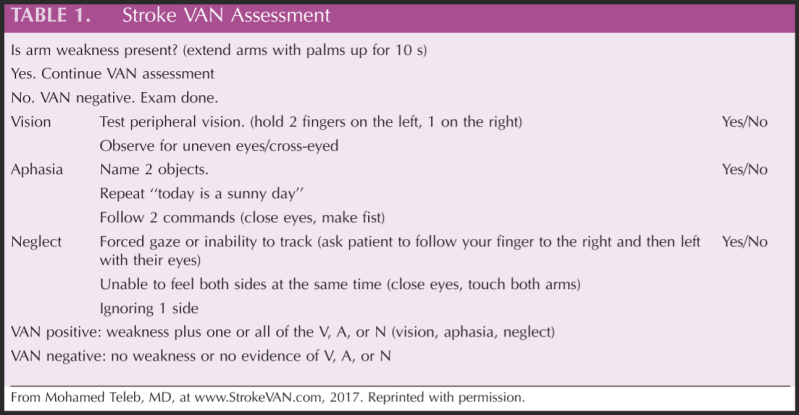
The VAN assessment is simple and easy to learn. It has a sensitivity of 100%, a specificity of 90%, and overall accuracy of 92% (Beume et al., 2018). These LVO exams also give you additional assessments to perform to identify a stroke. This is why they are the next step in evolving your stroke exam! But we have one more evolution to go thru....
Subtle Stroke/Stroke Syndromes
As you go through your career you will encounter several odd and atypical presentations of stroke (whether you realized it or not). It is crucial that we follow up on our patients so we can learn from those experiences. Your experiences, others experiences, training, and research are all a big part of evolving your stroke exam. This is how you will continue to improve and do those two things: identify the stroke and transport to the appropriate facility. In order to catch the subtle strokes you need a detailed exam that you have practiced and prepared over time. These exams will not be used on every patient, this is for the patient that is negative for a basic stroke exam and maybe even your LVO exam. You can think of these exams as focusing in on a specific area of the brain. Let's go through a few...
- Cerebellar Stroke Syndrome - This is a rare type of stroke. These patients usually have a chief complaint of: vertigo/dizziness, ipsilateral ataxia (falling to one side, fine motor skills), nausea/vomiting, and various sensation deficits (Yartsev, n.d.). Exams you can perform include: checking for nystagmus, dysmetria using the finger to nose test, and dysdiadochokinesia by asking patient to perform rapid alternating movements. Here is a video on assessing for cerebellar stroke.

- Anton Syndrome - This stroke usually involves the posterior cerebral artery and when thinking about that area of the brain we can expect vision deficits, specifically cortical blindness (Das, 2022). These patient's are considered to have Anton Syndrome when they are unaware of the blindness, which is called anosognosia (Das, 2022). The fact that they are unaware of their blindness makes it more difficult to identify. Watch how they move and listen closely to what they say. I have had one patient with Anton Syndrome and they often will argue that their vision is normal. For example, "yeah it's normal, I wear bifocal glasses and left them at home." Exams you can perform: central and peripheral vision check, ask them to follow your finger with just their eyes. The patient will have such severe vision loss that they may reach out to feel what is in front of them or even perform simple movements (walking) slowly as if they are unsure of their footing.
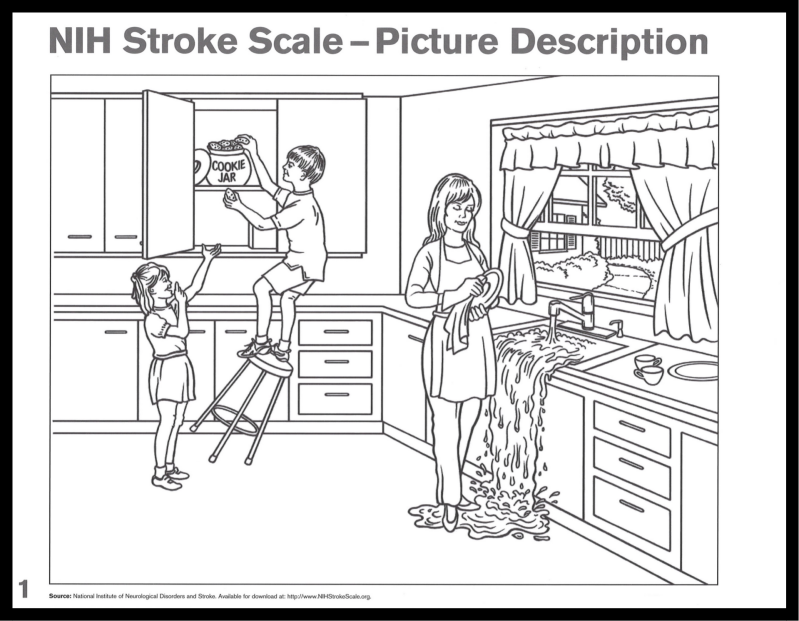
- Balint Syndrome - This stroke also involves the posterior cerebral artery, usually on both sides of the brain (Yartsev, n.d.). In this type of stroke the patient has difficulty with voluntary eye movements, optic ataxia, and asimultagnosia (inability to recognize visual objects). Exams you can perform: the finger to nose exam (patient will have difficulty touching objects away from body), ask patient to track your finger from side to side (patient has difficult tracking object), show patient an object or picture (they can identify one part of picture or one object but not multiple or see the whole picture). Here is a video on assessing for Balint Syndrome.
This last evolution is unique to you, make it yours! Your stroke exam should evolve over time and my hope is this blog gives you some guidance on where to begin. Lastly, I want to leave you with some final tips:
- Once we have identified the stroke and the most appropriate stroke facility there is no need to continue with the rest of the exam; time is brain.
- It is worth the time to do an detailed stroke assessment IF it helps identify a stroke.
- Your basic stroke exam is not good enough to identify some strokes. EVOLVE.
- Transport to a comprehensive stroke center when: we are outside window for tPA OR have signs of a large vessel occlusion (LVO).
- Follow up on your patient; you will be surprised what you'll learn.
- Watch other providers perform their stroke exam and use it to evolve your own.
- Ask the physician and neurologist questions.
- It is okay to be wrong; do not hesitate to call a stroke alert.
Take Care,
Tyler
References:
Beume LA, Hieber M, Kaller CP, Nitschke K, Bardutzky J, Urbach H, Weiller C, Rijntjes M. Large Vessel Occlusion in Acute Stroke. Stroke. 2018 Oct;49(10):2323-2329. doi: 10.1161/STROKEAHA.118.022253. PMID: 30355088.
Das, J. M. (2022, May 8). Anton Syndrome. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538155/
Haussen DC, Lima FO, Bouslama M, Grossberg JA, Silva GS, Lev MH, Furie K, Koroshetz W, Frankel MR, Nogueira RG. Thrombectomy versus medical management for large vessel occlusion strokes with minimal symptoms: an analysis from STOPStroke and GESTOR cohorts. J Neurointerv Surg. 2018 Apr;10(4):325-329. doi: 10.1136/neurintsurg-2017-013243. Epub 2017 Aug 2. PMID: 28768820.
Khaku, A. S. (2022, August 8). Cerebrovascular Disease. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK430927/
Starke, Robert M MD, MSc; McCarthy, David BS; Komotar, Ricardo J MD; Connolly, E Sander MD. Mechanical Thrombectomy for Stroke Effective Within 24-hour Window. Neurosurgery 82(5):p E107-E108, May 2018. | DOI: 10.1093/neuros/nyy046
Yartsev, A. (2022, May 27). Classical stroke syndromes. Deranged Physiology. Retrieved April 19, 2023, from https://derangedphysiology.com/main/required-reading/neurology-and-neurosurgery/Chapter%201501/classical-stroke-syndromes


Add comment
Comments